Neurologists and psychiatrists operate in two distinct fields within healthcare, yet their relationship is undeniably intertwined. Both focus on the brain and nervous system, addressing disorders that influence cognition, behavior, and emotion. Here’s how the overlap of these two fields provides valuable insights into understanding human health:
Both Fields Involve the Nervous System
At their core, both neurology and psychiatry focus on the nervous system. Neurology primarily examines the structural and functional aspects of the brain, spinal cord, and nerves. Psychiatric care, in contrast, looks at the same system through the lens of thoughts and behavioral changes. This connection underscores the biological basis of psychiatric conditions, shifting the perspective from mere psychological issues to a deeper neurological understanding.
Shared Symptoms and Diagnostic Challenges
One clear intersection between these fields lies in overlapping symptoms. For example, neurological conditions such as Parkinson’s disease, multiple sclerosis, or epilepsy frequently come with behavioral symptoms. Similarly, psychiatric disorders like schizophrenia or mood disorders can manifest with physical symptoms tied to the nervous system, such as motor disturbances or sensory changes. This overlap makes diagnosing and managing these conditions a collaborative effort, often requiring input from both neurologists and psychiatrists.
Neurotransmitters and Their Role
Neurotransmitters act as a bridge between the two specialties. These chemical messengers regulate vital brain functions, influencing mood, decision-making, and behavior. Dysfunctions within neurotransmitters, such as serotonin, dopamine, or norepinephrine, are linked to conditions like depression, anxiety, and even neurological disorders like Parkinson’s disease. By studying these messengers, neurologists and psychiatrists gain insights into both the biological and psychological patterns of various conditions.
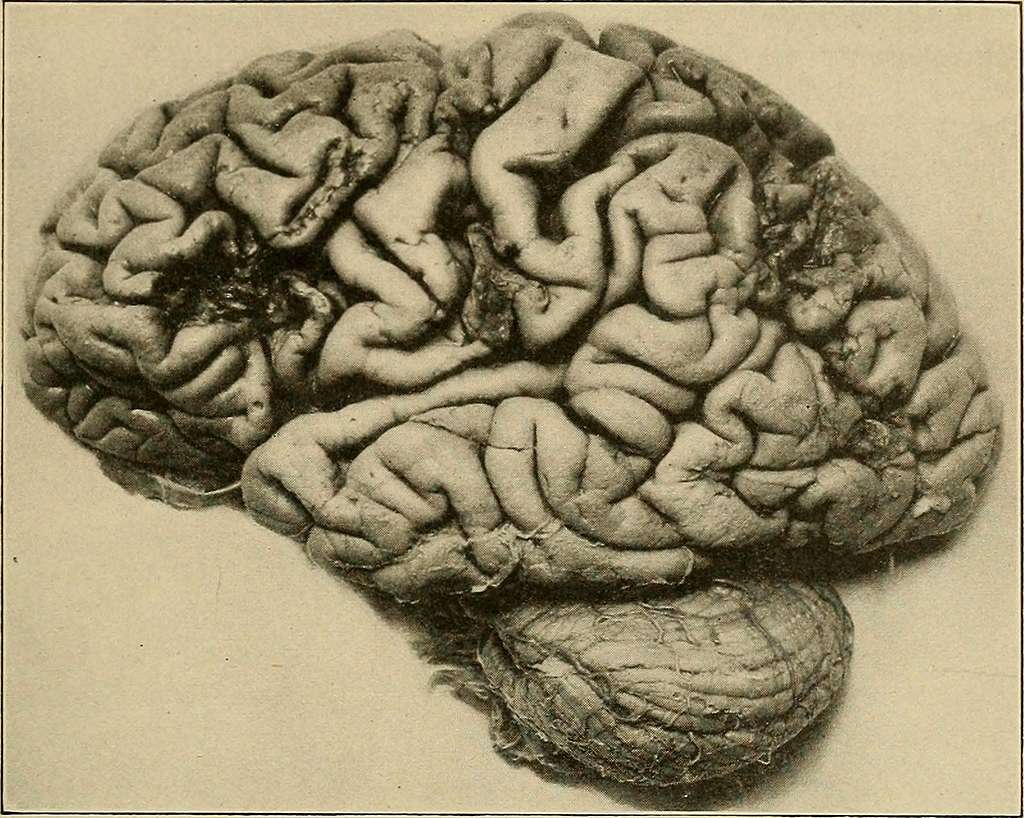
Brain Imaging Techniques in Psychiatry
Advancements in brain imaging technologies have deepened the connection between neurology and psychiatry. Tools such as MRI, PET scans, and fMRI reveal structural and functional changes in the brain linked to psychiatric disorders. For instance, researchers have identified differences in brain activity patterns in individuals with bipolar disorder or schizophrenia. These visual insights not only aid diagnoses but also tailor treatments by pinpointing areas of concern within the brain.
Genetics in Mental and Neurological Health
Genetics and environmental factors play a pivotal role in shaping both neurological and psychiatric conditions. Studies reveal that certain genetic predispositions may increase an individual’s likelihood of developing disorders like Alzheimer’s disease, ADHD, or schizophrenia. Meanwhile, environmental elements such as trauma, lifestyle, or stress may interact with these biological factors, contributing to the complexity of these disorders.
This interplay between genetics and environment challenges professionals in both disciplines to collaborate. Such a partnership creates a more holistic approach. It addresses the root cause of conditions while factoring in their broader impact on an individual’s life.
Ask Neurologists for More Information
While neurology and psychiatry are distinct, their interconnected paths point to the need for integrated care. Collaborative approaches pave the way for deeper understanding, more accurate diagnoses, and more effective treatments. Brain science continues to evolve, emphasizing the importance of addressing neurological and psychiatric health together as part of the same intricate system. Ask a neurologist for more information about how neurology and psychiatry are connected.
- mylovelyfurryfriend discover expert tips on dog health
- Infectious Diseases Updates – Stay Informed, Stay Protected!
- Wegovy For Weight Loss – A Breakthrough in Managing Obesity!
- Emergency Medicine Forum – A Hub for Fast-Paced Knowledge, Support & Updates!
- Pediatrics Discussions – Insights, Challenges, and Expert Advice for Better Child Health!



Leave a Reply